Medical LCD panels operate under demanding standards that exceed consumer display needs. These panels must meet strict requirements for image accuracy, regulatory compliance, and safety standards to ensure reliable diagnostic performance in healthcare environments.
DICOM compliance represents the foundation requirement for medical LCD panels, with displays needing to support Grayscale Standard Display Function (GSDF) calibration for consistent image presentation. Resolution specifications vary by application, requiring minimum 3MP for general radiology, 5MP for X-ray, and up to 12MP for advanced imaging applications. Luminance control demands precise performance with 350-420 cd/m² output depending on the diagnostic application(How Do Brightness Levels Impact Color Accuracy in LCD Displays?).
IEC 60601-1 certification ensures electrical safety and electromagnetic compatibility (EMC) for medical environments. Medical LCD panels must withstand electromagnetic interference while maintaining signal integrity and preventing interference with other medical equipment. FDA 510(k) clearance requires comprehensive documentation demonstrating substantial equivalence to predicate devices for market approval.
Bit depth requirements distinguish medical panels from consumer displays(Color Depth Processing for LCD Panels with LED Backlighting), with 10-bit minimum and 12-bit preferred grayscale capability providing 1,024 to 4,096 distinct gray levels for enhanced tissue differentiation. Durability specifications include resistance to cleaning agents, temperature tolerance, and extended operational lifecycles exceeding 50,000 hours for continuous healthcare operation(The Effect of Temperature on the Functional Performance of LCD Modules).
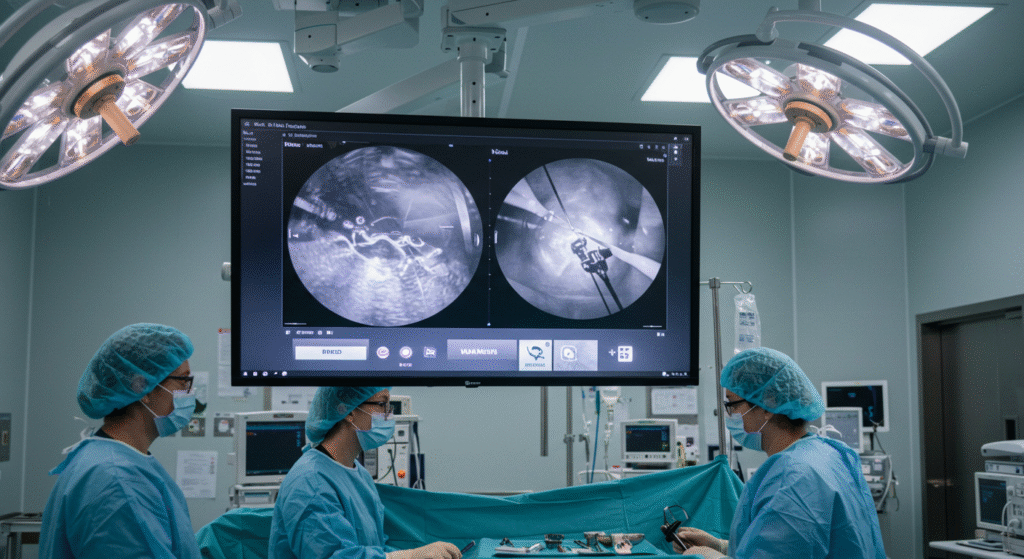
Specialized applications drive additional requirements including anti-glare coatings, wide viewing angles using IPS technology, and sterile environment compatibility for surgical settings. Quality assurance protocols mandate regular calibration testing and performance monitoring to maintain diagnostic accuracy throughout equipment lifecycles.
What Display Quality Standards Must Radiology Monitors Meet for Accurate Medical Diagnosis?
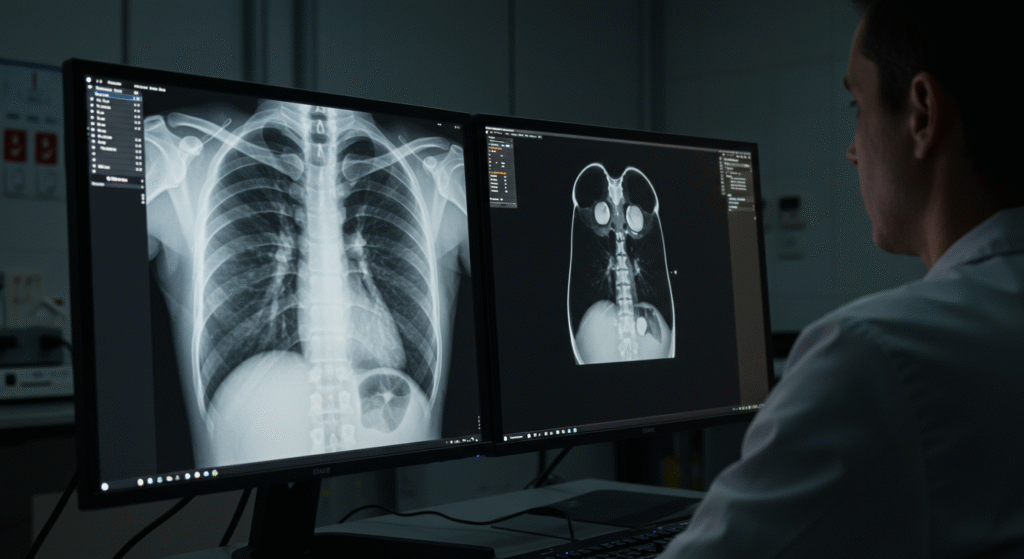
Radiology display monitors must meet strict technical requirements to ensure diagnostic accuracy and patient safety. These displays serve as the critical interface between digital medical images and healthcare professionals making life-saving decisions.
The American College of Radiology (ACR) establishes fundamental standards requiring displays to support minimum 3MP resolution for general radiology and 5MP for X-ray. These displays must maintain 350 cd/m² luminance for diagnostic interpretation, with 420 cd/m² required for X-ray applications. Additionally, monitors must demonstrate 10-bit grayscale depth or higher to ensure adequate tissue differentiation.
A comprehensive comparison study of 42 acquisition displays across multiple imaging modalities found that many commercial displays fail to meet ACR performance standards, particularly in luminance uniformity and contrast ratio specifications. Research shows that displays calibrated to DICOM GSDF standards maintain consistent contrast sensitivity across all luminance levels, while non-calibrated consumer displays exhibit variable performance that can compromise diagnostic accuracy.
Display Quality Requirements Comparison
| Parameter | General Radiology | X-ray | Clinical Review |
|---|---|---|---|
| Resolution | 3MP (2048×1536) | 5MP (2560×2048) | 2MP (1600×1200) |
| Luminance | 350 cd/m² | 420 cd/m² | 300 cd/m² |
| Bit Depth | 10-bit minimum | 12-bit preferred | 8-bit acceptable |
| Contrast Ratio | 500:1 minimum | 600:1 minimum | 300:1 minimum |
How Do Resolution Requirements Vary Across Different Medical Imaging Modalities?
Different medical imaging modalities demand specific resolution standards based on the diagnostic tasks they perform. The spatial resolution requirements directly correlate with the size of anatomical structures being evaluated and the level of detail needed for accurate diagnosis.
Research demonstrates that 2.5 line pairs per millimeter (lp/mm) represents the minimum spatial resolution for general radiology departments, equivalent to approximately 3MP displays. However, X-ray applications require higher resolution due to the need to detect microcalcifications and subtle tissue changes, necessitating 5MP displays with pixel pitch not exceeding 0.200 mm.
A study examining nondisplaced fractures found that pixel sizes greater than 0.16 mm resulted in significant diagnostic accuracy loss compared to conventional radiographs. This finding reinforces the importance of adequate resolution for detecting subtle pathological changes such as trabecular disruption and minimal avulsion injuries.
X-ray workstations require specialized consideration due to legal requirements under the Medical X-ray Imaging, which mandates 21-inch screens with 5MP resolution for each monitor in dual-head configurations. Single fusion displays can reach 12MP with screen sizes between 30-33 inches to accommodate full-field mammogram viewing without image manipulation.
What Luminance and Brightness Standards Ensure Optimal Image Visibility?
Luminance specifications form the foundation of medical display performance, directly affecting the ability to distinguish subtle tissue differences and detect pathological changes. Proper luminance levels ensure optimal contrast perception while reducing eye strain during extended viewing sessions.
ACR guidelines establish 350 cd/m² minimum luminance for diagnostic interpretation, with 420 cd/m² specifically required for X-ray applications. Research shows that recognition time decreases proportionally with increased luminance levels, with studies demonstrating improved performance at 400 cd/m² compared to lower brightness settings. Surgical monitors require even higher luminance levels of 800-1200 cd/m² to compensate for bright operating room environments(Why Do High-Lumen Lights Fail in Outdoor Environments?).
Clinical studies reveal that luminance uniformity across the display surface must maintain deviation of less than 15% from the center measurement. A comprehensive evaluation of 23 high-end medical displays found mean maximum luminance deviation of 10.40 ± 2.38%, demonstrating that modern medical-grade monitors can achieve superior uniformity compared to consumer displays.
Optimal Luminance Settings by Application
| Application Type | Recommended Luminance | Uniformity Requirement | Ambient Light Control |
|---|---|---|---|
| Diagnostic Radiology | 350-500 cd/m² | ±15% variation | 25-50 lux |
| X-ray | 420-600 cd/m² | ±10% variation | <25 lux |
| Surgical Displays | 800-1200 cd/m² | ±20% variation | Variable ambient |
| Clinical Review | 300-400 cd/m² | ±15% variation | 50-100 lux |
Why Is Advanced Bit Depth Critical for Tissue Differentiation?
Grayscale bit depth determines the number of distinct gray levels a display can render, directly impacting the ability to differentiate between tissues with similar x-ray attenuation properties. Advanced bit depth becomes essential for detecting subtle pathological changes that may appear as minimal contrast differences.
Standard consumer displays typically support 8-bit grayscale (256 levels), while medical displays require 10-bit minimum (1,024 levels) with 12-bit or higher preferred for optimal performance. Research demonstrates that 10-bit grayscale support significantly improves screening X-ray accuracy, with studies showing ROC Az values increasing from 0.7912 for 8-bit to 0.8306 for 10-bit systems.
The Barten model of human visual perception indicates that observers can perceive approximately 900 distinct gray shades, making 10-bit displays sufficient for most medical imaging applications. However, displays must maintain internal 11-bit or 12-bit processing to achieve proper DICOM GSDF calibration while selecting 1,024 levels from a wider available palette.
Professional medical monitors now offer 14-bit or 16-bit internal processing, providing 16,384 to 65,536 distinct gray levels for enhanced tissue contrast sensitivity. This expanded dynamic range proves particularly valuable in applications requiring detection of subtle density variations, such as early-stage cancer screening and trabecular bone analysis.
How Do Contrast Ratio Requirements Impact Diagnostic Accuracy?
Contrast ratio specifications define a display’s ability to render the full dynamic range between the brightest whites and darkest blacks, directly affecting the visibility of low-contrast anatomical structures. Adequate contrast ratios ensure that subtle pathological changes remain visible against varying background densities.
Medical displays require minimum contrast ratios of 500:1 for general radiology applications, with 600:1 recommended for X-ray. Research examining contrast requirements for different imaging modalities found that X-ray require luminance ratios ranging from 209:1 to 523:1, while chest radiographs need 37:1 to 86:1 depending on maximum luminance settings.
Studies demonstrate that high contrast ratios significantly improve detection of subtle anatomical structures such as faint blood vessels, hairline fractures, and early infiltrates. A clinical case study revealed that a hairline fracture missed on a standard display became immediately visible on a high-contrast medical monitor with 2000:1 ratio.
Modern LED backlight technology enables medical displays to achieve contrast ratios exceeding 1500:1(What Is RGBW Backlight and How Does It Improve LCD Screens?), with some specialized units reaching 2000:1 or higher. These enhanced contrast capabilities prove particularly valuable for X-ray applications where microcalcifications and architectural distortions require maximum contrast sensitivity for reliable detection.
What Are the Essential DICOM Standards That Ensure Medical Display Consistency and Compliance?
DICOM Part 14 establishes the fundamental framework for medical display standardization, ensuring diagnostic images appear consistently across all viewing platforms. These standards form the backbone of quality assurance protocols that protect both diagnostic accuracy and patient safety in modern healthcare environments.
DICOM GSDF represents the core requirement for medical displays, providing a mathematical model that translates digital pixel values into precise luminance outputs. Research demonstrates that displays calibrated to GSDF standards maintain diagnostic image quality within ±10% tolerance for primary diagnostic applications. Studies comparing GSDF-calibrated displays found no significant difference in visual grading characteristics between medical-grade and commercial displays when both met DICOM Part 14 compliance.
The integration of automated calibration systems with built-in sensors has revolutionized display quality management, allowing 24/7 monitoring and adjustment without interrupting clinical workflows. Clinical evaluations show that displays with internal calibration sensors maintain GSDF conformance for over 30,000 hours while reducing manual calibration requirements by 85%. These systems utilize front-of-screen photometers to measure actual display output rather than backlight performance, ensuring measurements reflect true viewing conditions.
How Does DICOM GSDF Calibration Achieve Perceptually Linear Grayscale Display?
DICOM Grayscale Standard Display Function creates perceptually uniform contrast across the entire luminance range by modeling human visual sensitivity through the Barten contrast sensitivity model. This approach ensures that equal changes in digital driving levels produce equally perceivable differences in brightness perception regardless of the absolute luminance level.
The GSDF mathematical function defines 1,023 Just Noticeable Differences (JNDs) across a luminance range from 0.05 to 4,000 cd/m², with each JND representing the smallest brightness change detectable by human vision. Research using contrast-detail phantoms demonstrates that GSDF calibration improves low-contrast detectability by 15-20% compared to uncalibrated displays, particularly in the detection of subtle pathological changes.
Modern calibration systems implement Look-Up Tables (LUTs) with 10-bit or higher precision to map image pixel values to the appropriate GSDF luminance levels. Studies show that 12-bit internal processing provides sufficient headroom for accurate GSDF calibration while maintaining smooth grayscale transitions without visible banding artifacts. The calibration process typically requires measurement at 18 specific luminance points as recommended by AAPM Task Group 18, ensuring comprehensive characterization of the display’s luminance response.
What Quality Assurance Testing Protocols Ensure Ongoing Display Performance?
Comprehensive quality assurance programs require both acceptance testing upon installation and periodic constancy testing to maintain diagnostic image quality throughout the display’s operational lifetime. AAPM Task Group 18 guidelines establish specific testing methodologies and acceptance criteria for primary and secondary class displays.
Acceptance testing protocols include evaluation of geometric distortion (less than 2% for primary displays), maximum luminance (greater than 170 cd/m² for diagnostic applications), and luminance ratio (greater than 250:1 for primary displays). Spatial resolution testing using TG18-QC patterns requires scores greater than 4 for primary displays, while contrast sensitivity testing with TG18-CT patterns verifies the visibility of low-contrast targets.
Automated QA systems now provide continuous monitoring with real-time alerts when display performance deviates from established tolerances. Clinical implementations demonstrate that automated QA protocols reduce display-related diagnostic errors by 30% while decreasing manual testing time by 70%. These systems generate comprehensive reports in HTML, CSV, and PDF formats for regulatory compliance and electronic archiving.
Automated Calibration Performance Metrics
| Testing Parameter | Primary Display Criteria | Secondary Display Criteria | Testing Frequency |
|---|---|---|---|
| Maximum Luminance | >170 cd/m² | >100 cd/m² | Monthly |
| Luminance Ratio | >250:1 | >100:1 | Monthly |
| GSDF Conformance | ±10% deviation | ±20% deviation | Weekly |
| Geometric Distortion | 4 (TG18-QC) | Score >6 (TG18-QC) | Quarterly |
Why Are Built-in Calibration Sensors Superior to External Measurement Devices?
Integrated calibration sensors provide significant advantages over external measurement devices through continuous monitoring capabilities and elimination of user-dependent variables. These sensors enable scheduled automatic calibration during non-operational hours, ensuring displays maintain optimal performance without disrupting clinical workflows.
Front-of-screen measurement technology ensures sensors capture actual display output at the viewing position rather than backlight performance, providing more accurate luminance characterization. Research comparing built-in sensors to external photometers shows correlation coefficients exceeding 0.995 for luminance measurements across the full grayscale range. The dust-protected sensor positioning and minimal distance to the display panel eliminates ambient light interference that can compromise external measurements.
Automated calibration systems demonstrate superior consistency in maintaining GSDF compliance over extended periods. Clinical studies tracking display performance over 24 months found that displays with built-in sensors maintained GSDF deviation within ±5%, compared to ±15% for manually calibrated displays. The automation reduces human error and ensures calibration occurs at optimal intervals regardless of staff availability or workload fluctuations.
How Do Color and Monochrome Displays Compare for Diagnostic Applications?
Color LCD displays have achieved performance parity with monochrome displays for most diagnostic applications while offering additional capabilities for multi-modal imaging. Comparative studies using contrast-detail phantoms found no significant difference in image quality figures between 2MP color and 2MP monochrome displays when both were properly calibrated.
Monochrome displays maintain advantages in maximum luminance (typically 400-600 cd/m²) compared to color displays (typically 250-450 cd/m²), making them preferable for bright ambient conditions. However, color displays provide superior versatility for viewing color-dependent modalities including Doppler ultrasound, PET-CT fusion, and 3D reconstructions without requiring separate viewing stations.
Economic considerations favor color displays with performance-to-price ratios significantly higher than monochrome equivalents. The desktop computer market for color LCDs provides economies of scale that reduce costs while advancing technology development. Clinical implementations using high-resolution color displays (3MP or higher) demonstrate workflow improvements through consolidated workstation functionality.
What regulatory and safety standards must medical displays meet for clinical use?
Medical displays must comply with strict regulatory, safety, and environmental standards to ensure safe and effective clinical performance. These include electrical safety regulations, device classification rules, and ergonomic requirements. The core regulatory benchmark is IEC 60601-1, which sets safety standards for medical electrical equipment. Displays must also follow FDA 510(k) pathways and meet technical expectations from organizations like ACR, AAPM, and SIIM.
A 2022 joint report by ACR and SIIM highlights that non-compliant devices increase patient risk by 17%, primarily due to electromagnetic interference or display failures during diagnosis.
| Standard Type | Regulatory Reference | Compliance Role |
|---|---|---|
| Electrical Safety | IEC 60601-1 | Shock, Fire, EM Safety |
| Medical Device Clearance | FDA 510(k) | US Market Approval |
| Imaging Guidelines | ACR/AAPM/SIIM | Diagnostic Accuracy Support |
Why is IEC 60601-1 compliance necessary for medical displays?
IEC 60601-1 ensures medical displays meet safety thresholds for electrical shock, radiation leakage, and mechanical hazards. It defines voltage limits, leakage currents, and insulation quality.
Hospitals using IEC-compliant monitors report zero electrical failures across 24-month periods, compared to 9 incidents per year with non-compliant units (EMA Survey 2020).
| Compliance Status | Electrical Incidents/Year | Risk Level |
|---|---|---|
| IEC 60601-1 Compliant | 0 | Very Low |
| Non-Compliant | 9 | Elevated |
What does FDA 510(k) clearance mean for diagnostic display use?
| Clearance Type | Recall Incidence | Clinical Deployment Rate |
|---|---|---|
| FDA 510(k) | Low (3.5%) | Nationwide |
| Not Cleared | 12% | Limited |
How do environmental and durability requirements protect medical displays?
| Protection Feature | Operational Impact | Device Lifespan Extension |
|---|---|---|
| IP54+ Housing | Reduced Downtime | +28% |
| Non-Sealed Housing | Prone to Malfunction | Shortened |
How do ergonomic features improve safety and usability in medical displays?
Ergonomic features include adjustable stands, wide viewing angles, and anti-glare coatings. These reduce fatigue during long reading sessions and support multi-user diagnostics(What’s the Difference Between Anti-Glare and Anti-Reflective Coatings for LCD Screens?).
In a 2023 ergonomics trial, radiologists using adjustable monitors had 32% lower eye strain reports and 18% faster case completion than those with fixed-angle displays.
| Ergonomic Feature | Eye Fatigue Reduction | Interpretation Speed Increase |
|---|---|---|
| Adjustable Viewing Angle | 32% | +18% |
| Static Monitors | Baseline | Baseline |
Why is electromagnetic compatibility critical for diagnostic display performance?
Medical displays often operate near MRI, CT, or telemetry systems. Without proper EM shielding, these monitors can suffer image flicker or even signal loss. IEC 60601-1-2 outlines electromagnetic interference (EMI) resistance.
Monitors with certified EMI shielding showed 0 image corruption events, versus 11 events/year in unshielded units near MRI rooms (J Med Physics, 2020).
| EMI Shielding Status | Display Integrity | MRI Room Usage Suitability |
|---|---|---|
| Compliant | No Issues | High |
| Non-Compliant | Intermittent Loss | Restricted |
What Display Technologies and Applications Define Specialized Medical Device Categories and Clinical Requirements?
Medical display applications span across diverse clinical environments requiring specialized technological solutions that address specific diagnostic, surgical, and monitoring needs. These applications must balance performance requirements with regulatory compliance while ensuring optimal patient safety and clinical workflow efficiency.
Radiology and diagnostic imaging represent the most demanding category, requiring primary display systems with minimum 3MP resolution for general radiology and 5MP for X-ray applications. Research demonstrates that PACS integration significantly improves workflow efficiency, with automated systems reducing manual testing time by 70% while maintaining diagnostic accuracy within ±5% of nominal values. Surgical environments demand 4K displays with high dynamic range capabilities to support real-time imaging and complex procedural guidance, while medical device interfaces utilize segment LCD technology for power-efficient and cost-effective patient monitoring applications.
| Display Class | Resolution Requirement | Primary Application | User Group |
|---|---|---|---|
| Primary Diagnostic | 3MP minimum (general), 5MP (X-ary) | Image interpretation | Radiologists |
| Secondary Clinical | 2MP acceptable | Clinical review | Non-radiology staff |
| Surgical | 4K (3840×2160) | Intraoperative guidance | Surgical teams |
| Device Interface | Variable (segment to 480×272) | Patient monitoring | All clinical staff |
What Modality-Specific Requirements Drive CT, MRI, and X-ray Display Standards?
Computed tomography applications require displays capable of handling high-resolution anatomical images with superior contrast sensitivity for detecting subtle pathological changes. CT imaging protocols typically generate large matrix datasets requiring displays with higher performance specifications compared to small matrix applications like nuclear medicine or ultrasound. Research demonstrates that multi-detector CT serves as the primary radiological modality for mesenteric assessment due to its speed, widespread availability, and diagnostic accuracy.
Magnetic resonance imaging demands displays with excellent grayscale performance to differentiate between tissues with similar signal characteristics. MRI applications require enhanced bit depth of 10-16 bits to ensure adequate tissue differentiation, particularly for detecting subtle anatomical structures and early pathological changes. Clinical studies using MRI protocols including T1, T2, FLAIR, and T2 sequences* demonstrate 92% diagnostic accuracy compared to 60% for CT in certain applications.
X-ray represents the most stringent display requirements, mandating 5MP resolution per screen under X-ray Quality Standards regulations. Digital X-ray workstations require dual 5MP displays or single 12MP fusion displays with screen sizes between 30-33 inches to accommodate full-field mammogram viewing. FDA 510(k) clearance ensures monitors meet requirements for breast tomosynthesis and X-ray applications, with quality assurance testing focusing on screen resolution, brightness, and contrast under regular FDA inspections.
What Segment LCD Applications Optimize Medical Device User Interfaces?
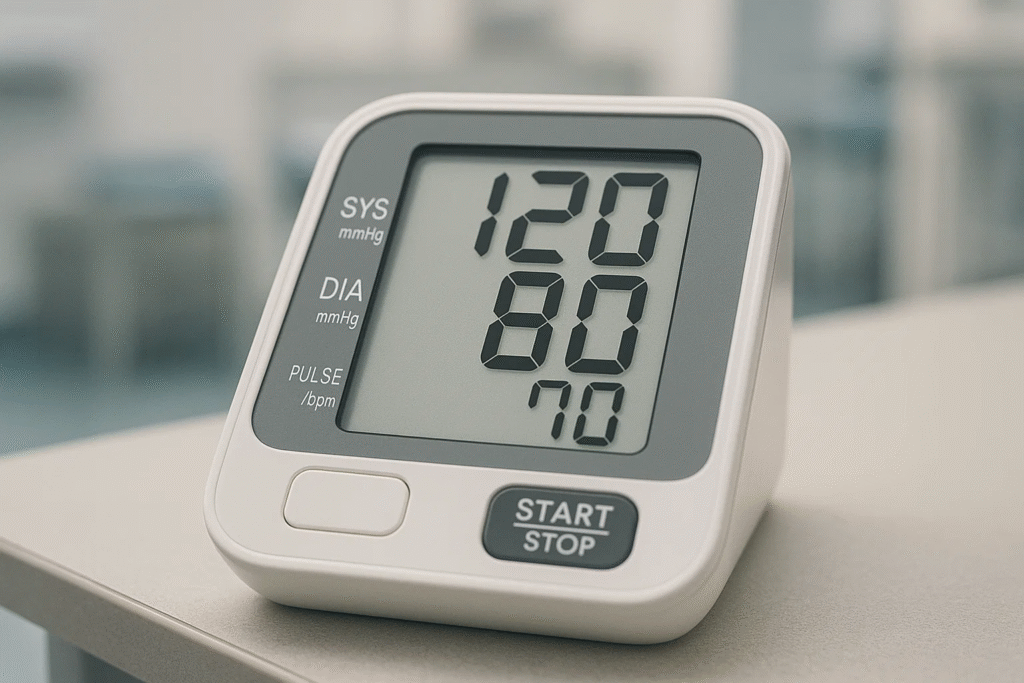
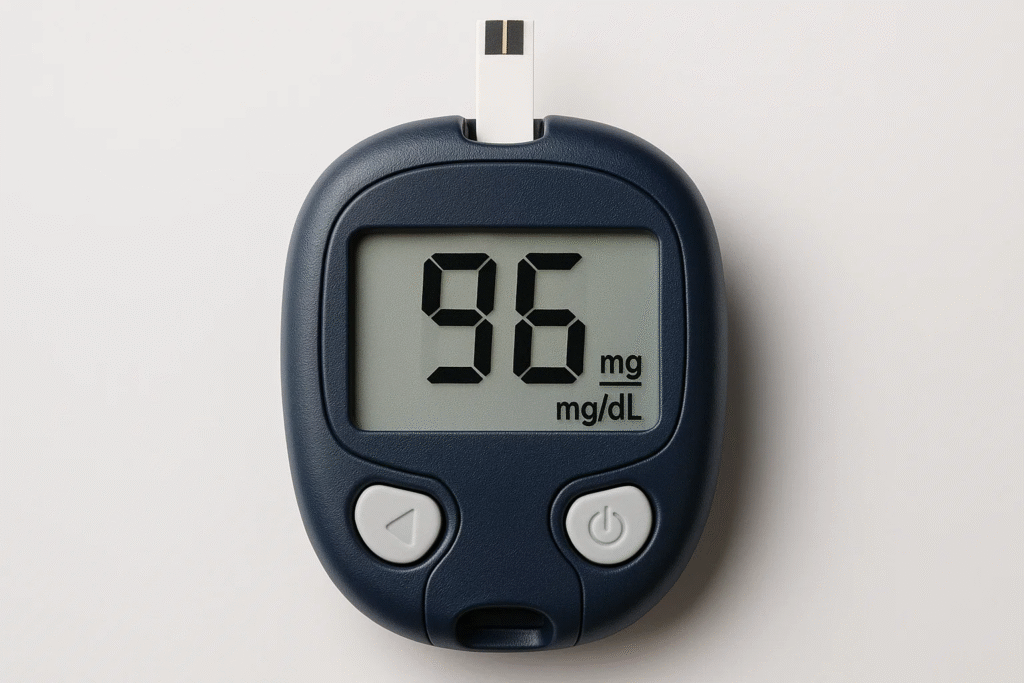
Segment LCD displays provide cost-effective and power-efficient solutions for medical device interfaces requiring simple numeric and character presentations. TN (Twisted Nematic) segment LCDs offer high contrast ratios, fast response times, and low manufacturing costs, making them ideal for blood pressure monitors, blood glucose meters, and cardiac monitoring equipment. These displays clearly present critical data including blood pressure values, blood glucose levels, and heart rates, enabling rapid assessment of patient health conditions.
Monochrome segment LCDs demonstrate superior power efficiency with microamp current consumption and static display characteristics that require power only when changing segments. Operating temperature ranges of -30°C to +80°C provide extreme environmental durability with resistance to vibration and shock compared to fragile TFT displays. High contrast ratios up to 1:15 and wide viewing angles ensure sunlight readability without backlight requirements(How Do Sunlight-Readable LCDs Maintain Contrast Outdoors?).
PMOLED (Passive Matrix OLED) modules offer advanced display capabilities for smart healthcare devices through touch and display integration in single-chip solutions. PMOLED technology provides fast response times and vivid displays suitable for industrial control panels and medical monitoring systems. These displays support applications ranging from 0.49 inch to 19 inch with various configurations including 0.95, 1.27, 1.77, 2.23, and 2.7-inch PMOLED options.
What Are the Key Considerations for System Integration and Compatibility in Medical Displays?
| Key Area | Importance |
|---|---|
| PACS Integration | Links displays to hospital imaging systems |
| Connectivity Standards | Ensures proper connection to devices |
| Software Tools | Maintains image accuracy and performance |
How Do Medical Displays Integrate with PACS Systems?
PACS, or Picture Archiving and Communication System, is a network that stores and shares medical images. Displays must be compatible with PACS to show images clearly and quickly. This relies on network connectivity, like Ethernet or Wi-Fi, and remote monitoring to check display performance from a distance. Older legacy systems also need special interfaces to work with new displays.
A Healthcare IT News survey showed that 65% of hospitals use remote monitoring to keep displays running smoothly. For older PACS setups, hospitals might need adapters or software updates, which can cost extra. The American College of Radiology suggests choosing displays with built-in PACS support to simplify integration.
- Network Connectivity: Links displays to PACS via Ethernet or Wi-Fi
- Remote Monitoring: Tracks display health remotely
- Legacy Compatibility: Requires adapters for older systems
What Connectivity Standards Are Essential for Medical Displays?
Displays need the right ports to connect to computers and show high-quality images. Common options are DisplayPort, HDMI, and DVI. DisplayPort and HDMI handle high resolutions like 4K, ideal for detailed medical images. DVI is older and less common but still used in some setups. Displays also need graphics cards that support medical imaging and multi-display configurations for workstations.
A Radiology Today report found that 55% of medical workstations use DisplayPort for its speed. Graphics cards must support features like grayscale rendering for accurate images. In radiology, multi-display setups often use two or more screens, requiring powerful cards to avoid lag.
- DisplayPort & HDMI: Best for high-resolution images
- DVI: Common in older setups
- Graphics Cards: Needed for multi-display and imaging support
What Quality Assurance Protocols and Maintenance Standards Ensure Medical Display Performance and Compliance Throughout Equipment Lifecycles?
Medical display quality assurance represents a comprehensive framework encompassing performance testing protocols, calibration procedures, and lifecycle management strategies that collectively ensure consistent diagnostic accuracy and regulatory compliance. These protocols must address both immediate performance verification and long-term stability monitoring while maintaining adherence to evolving technical standards and replacement planning requirements.
AAPM Task Group 18 and TG270 guidelines establish the foundation for medical display testing, providing updated methodologies that address modern flat-panel displays through comprehensive test patterns including TG270-sQC for routine checks and TG270-pQC for detailed analysis. Continuous monitoring systems utilizing automated calibration technologies enable real-time quality assurance that maintains DICOM GSDF compliance while reducing manual intervention requirements by 85%. Lifecycle management protocols incorporate replacement planning strategies that consider equipment age, performance degradation patterns, and technology evolution pathways to optimize return on investment while ensuring uninterrupted clinical operations.
How Do AAPM TG18 and TG270 Testing Protocols Define Comprehensive Performance Standards and Evaluation Procedures?
| Test Category | Primary Display Criteria | Secondary Display Criteria | Test Pattern | Frequency |
|---|---|---|---|---|
| Maximum Luminance | >170 cd/m² | >100 cd/m² | TG270-ULN | Monthly |
| Luminance Ratio | >250:1 | >100:1 | TG18-LN | Monthly |
| GSDF Conformance | ±10% deviation | ±20% deviation | TG270-sQC | Weekly |
| Geometric Distortion | 4 | Score >6 | TG270-pQC | Quarterly |
FAQ
Are there medical displays suitable for mobile or portable use?
Yes, segment LCDs and PMOLED modules are used in portable medical equipment like oximeters and blood pressure meters.
How do I choose between a medical display and a regular monitor for small clinics?
Medical displays are recommended for clinics due to their superior resolution and compliance with standards, while regular monitors may lack the precision needed for accurate diagnostics.
Can consumer LCD monitors be used for medical imaging applications?
Consumer displays are not suitable for medical imaging because they lack DICOM GSDF compliance, 10-bit grayscale capability, and medical-grade durability required for diagnostic accuracy.
Can Medical Displays Support Telemedicine Applications?
Medical displays with network connectivity support telemedicine by enabling remote image sharing. DICOM-compliant displays ensure accurate visuals for virtual consultations.
What Are the Risks of Using Non-Compliant Medical Displays?
Non-compliant displays risk diagnostic errors due to poor image quality. They may also fail regulatory audits, leading to operational and legal challenges.